Verification process could be burdensome and result in coverage losses, critics warn
May 23, 2025
- House-passed bill would require 80 hours of monthly work or community engagement for Medicaid eligibility.
-
Experts warn that burdensome verification processes could result in millions of unintended coverage losses.
-
Even exempt individualslike caregivers or those with disabilitiesmay be swept into the reporting burden.
A sweeping tax and spending bill passed by House Republicans is raising alarms among health policy experts for its inclusion of a national Medicaid work requirement that could leave millions without coverageeven among groups meant to be exempt.
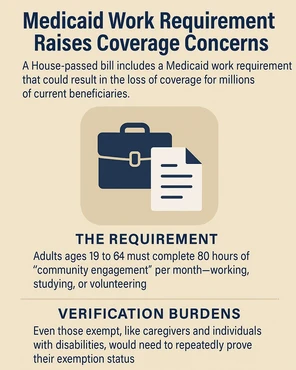
The proposed legislation, H.R. 1, seeks to generate nearly $273 billion in Medicaid savings by mandating that adults aged 19 to 64 log 80 hours of monthly community engagementthrough work, education, or community service. While the measure still awaits action in the Senate, researchers warn that the logistical and bureaucratic burden of verifying compliance or exemptions could cause many to fall through the cracks.
An analysis from the Urban Institute estimates that 5.5 to 6.3 million people could lose Medicaid coverage under this requirementthe most significant structural change to the program since the Affordable Care Act expanded access.
Exempt in theory, butin practice?
Though the bill includes exemptions for caregivers, parents, and individuals with disabilities or chronic conditions, these groups would still be required to periodically prove their exempt status. That means repeatedly navigating complex verification systems, filing paperwork, and potentially facing delays or denials that lead to temporary or permanent loss of benefits.
Even if people think the requirements are reasonable, they can end up hurting the people who now need to go through this process periodically, said Chiquita Brooks-LaSure, former CMS administrator.
The bill sets a deadline of December 31, 2026, for all states to begin verifying work or exemption status at the time of both enrollment and eligibility renewal. Employment history for the prior month must be confirmed, adding a layer of complexity that concerns advocates and researchers alike.
Lessons from Arkansas
Experts point to the 2018 Medicaid demonstration in Arkansas as a cautionary tale. The program, which enforced similar work rules, resulted in 18,000 people losing coverage in just nine monthsmany of whom should have been exempt but were tripped up by confusing and narrow reporting processes.
In that pilot, exemptions for people with substance use disorders or those caring for an incapacitated family member lasted only two months, requiring frequent re-verification. The burden of proofoften without adequate state guidanceleft many vulnerable beneficiaries unable to keep up.
How do you prove that youre caring for your sick mother? asked Leonardo Cuello, a research professor at Georgetown University. If the exemptions are too narrow, people with legitimate need will be excluded.
Administrative Burden Could Undermine Program Goals
Health policy leaders such as Robin Rudowitz of KFF emphasize that the bill lacks clarity on implementation, particularly around how states are to validate exemptions. While it allows for the use of employment databases, manual verification is still expected for many, especially among those who are self-employed, work informal jobs, or care for family members.
The underlying fear is that the administrative complexity of proving eligibilityrather than actual disqualificationwill result in large-scale disenrollment. Vulnerable groups may simply be unable to meet the documentation standards or deadlines.
A Call for Caution
As the bill heads to the Senate, advocates are calling for more thoughtful policy design, clearer federal guidance, and a serious reckoning with the human cost of bureaucracy.
This isnt just a policy issueits a public health crisis in the making, said Laura Harker of the Center on Budget and Policy Priorities.
#Medicaid #work #requirement #spell #trouble #vulnerable #groups